Hypo Guide
A hypo or hypoglycemia is an episode of low blood sugar (generally considered below 70 mg/dl) that mostly happens to diabetics on insulin or oral diabetes medication. Whether you're new to diabetes (read our tips for newly diagnosed families) or a veteran, hypo management is essential for all of us.
Hypos need to be treated immediately
Symptoms
- Shakiness
- Palpitations
- Sweating (or feeling hot or cold)
- Hunger
- Irritability (or marked changed in behaviour)
- Confusion
- Weakness, dizziness or nausea
- Clumsiness
- Blurred vision
Hypos can escalate quickly. If left untreated, they could lead to seizures, unconsciousness or in the worst case scenario, death.
How to treat a hypo
1.Check
You can't be sure that you have a hypo unless you confirm it on your glucometer. It doesn't make sense to only rely on the symptoms because they could be wrong. Some people might feel hypo (low) symptoms but actually be high. Some might feel hypo at normal sugars if their bodies are used to being high all the time. It is important to test first. Always carry your meter in your diabag or kit. Having said that, if you don't have access to your meter but feel a hypo, it's safer to just treat it.
2.Treat
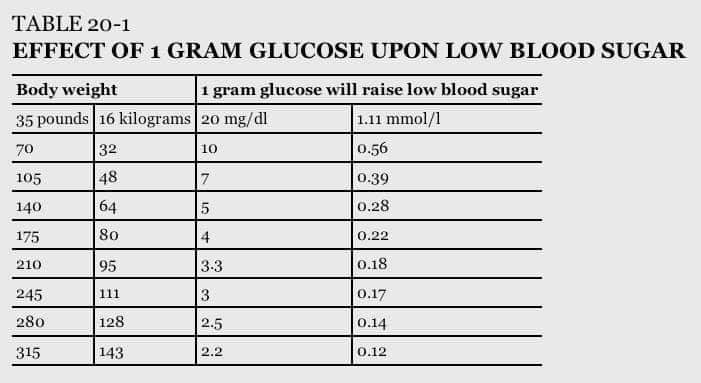
The ideal way to treat a hypo is with a measured amount of glucose or sugar (glucose powder or gel, glucose tablets like these or these, glucose or sugar water or sugar cubes, grains, or sachets). Everyone needs different amounts of glucose to bring them back to normal based on their current reading and sweeping generalizations don't work for all - for example, the commonly recommended 15gms of fast acting carbohydrate might be too much for a child or a carb sensitive adult. Here's a chart to help you understand how much would 1 gm glucose bring up your sugars based on body weight. Using this guideline, you can estimate by how many mg/dl would a glucose tab or spoonful of sugar bring you up.
In the worst case scenario that you don't have anything on you and are on the pump, you could suspend your pump for a little while (or do a 0% temporary basal) until your sugars start rising again.
3.Check again
It is imperative to test your BG again in about 15 minutes or so to know if your sugars are back in range and you're out of immediate danger.
Here's my two cents on treating hypos. See more #HypoHacks videos here.
Causes
- Too much insulin or medication (could be a wrong dose estimate or accidentally taking the wrong type of insulin)
- Too little food (for the insulin taken)
- Sudden rigorous exercise (without dose adjustment or a snack) - may cause delayed hypos. Read on exercise and BG here.
- A new regime without appropriate dose adjustment - of medication, food, exercise, weight loss
- Alcohol (certain kinds of alcohol combined with not eating)
- Other illnesses such as those related to the kidney or liver could cause hypos
- Hormonal deficiencies such as Addison's disease could cause hypos in non-diabetics too
Hypo unawareness
When you lose all symptoms of being in hypo, things can go downward (pun intended) because you may not know until it's dangerously low. Hypo unawareness happens if your body gets used to being too low all the time. The way to reverse it is to try staying in range and correcting hypos quickly.
Severe hypos, nocturnal hypos and Glucagon
Severe hypoglycemia is one where you need external help. If someone is drowsy, unconscious or not responsive, treat it as an EMERGENCY.
- Put them in a recovery position and don't feed if unconscious
- Administer a Glucagon injection (always keep one at home and learn how to use it as a caregiver)
- Call for help (an ambulance, family etc.) if they haven't recovered in 10 minutes
Nocturnal or night time hypos can be dangerous if you don't realize and are unable to wake up to treat it before it gets severe. Always test before sleeping. If you've done intense exercise, tweak your doses if needed. If possible, use a Continuous Glucose Monitor (CGM) or a Flash Glucose Monitor (FGM) to analyze trends.

Diabetic Alert Dogs (DADs)
Trained service dogs that can alert a T1 of an existing or oncoming hypo/hyper could be of additional help. There are organizations in several countries that train dogs. Certain people notice that their untrained pet dog or cat can also tell if they're in hypo. If you do have a pet, try and let us know if they can tell!
Here are some tips to help you avoid and navigate hypos and be fully prepared :
Dos
- Use a glucometer to ascertain hypos. Test your BG often in a day (before and after meals, exercise and bed).
- Treat hypos with glucose or sugar
- Use the Law of Small Numbers (Tip : being on low carb has actually reduced the number and severity of my hypos. Surprised? Read some keto/low carb myths)
- Test BG before going to bed (and in the middle of the night too, every once in a while)
- Carry a medical ID that clearly mentions you are an insulin dependent T1 and what to do incase of hypo.
- Always keep your meter and hypo treatment with you. Keep tabs in each bag, each room, at work, at the gym, in school, by your bed side, in the car - you do not want to be stuck without your life saving supplies!
- Correct basal - very important to ensure less hypos. Do a basal check and adjust if required.
- Let people around you know what to do incase of a hypo where you can't help yourself. Make an emergency plan and share it. Talk to your family, spouse, school teachers, room mates, friends, colleagues, relatives - whoever you spend time with.
- If you live alone, share your BG data with someone. Have a network of friends/family/neighbours who can be responsible and check up on you if you don't respond.
- Always log your hypos, especially if they are frequent and discuss with your medical professional to look for solutions.
Don'ts
- Don't treat hypos with food. Sure, you could have a small protein rich snack after glucose, if you feel hungry.
- Do not over correct, it can be a vicious circle. Rebound hypers and hypos are completely avoidable. It is very tempting to over eat or choose the wrong kind of foods and make hypos an 'excuse' to eat anything. It will be a regrettable decision BG wise and will add additional, unnecessary body weight. (Tip : I never treat my hypos in the kitchen to avoid temptation. I keep glucose tabs everywhere else)
- Chocolate (or cake, mithai etc) is not going to help a hypo quickly. The fat content in these foods will delay the absorption of glucose in the bloodstream making it longer and more dangerous to recover.
- Do not attempt to feed someone if they are unconscious. They could choke and die. (Tip : Rub glucose paste or gel on the inside of their cheeks or gums)
- Do not drive or operate machinery if you feel hypo and until you're back to normal.
- Don't mix up your bolus and basal pens or syringes (that could lead to a big hypo!). Keep them separately or mark them differently.
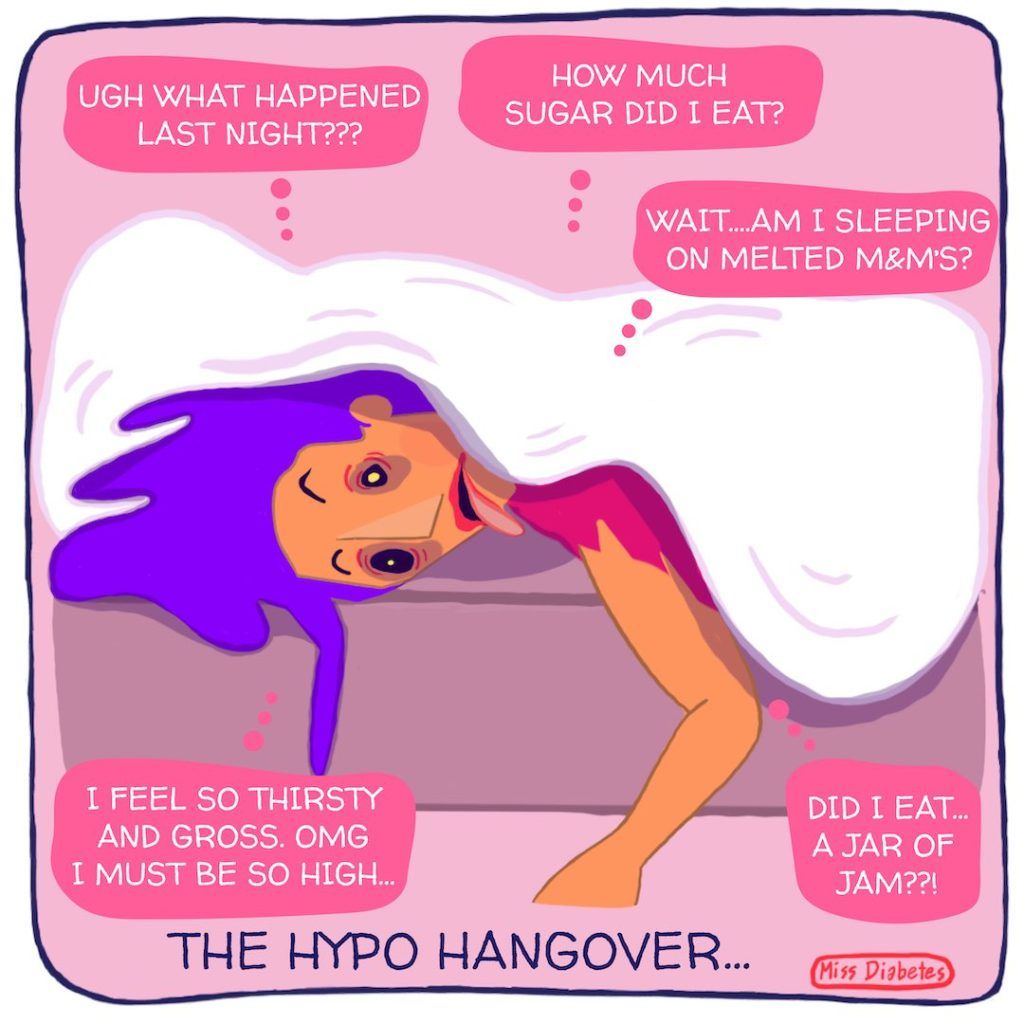
It's not easy being T1 or walking the tight rope between hypos and hypers, especially when you get a hypo hangover sometimes! If you don't know what that is, read our fun compilation of T1 words here and don't forget to check your BG!
SUPPORT BLUE CIRCLE DIABETES FOUNDATION
We need your help and support to continue to grow, expand and touch the lives of countless people in the diabetic community. Every little bit helps us in sustaining this endeavour.
Click here to donate