Sick day management with diabetes
*Disclaimer : This article is not intended as replacement for medical advice, please consult your healthcare professional when in doubt. This is the author's opinion, based on her experience of living with type 1 diabetes for 25 years.
Being ill is no fun for anyone. Managing the ins and outs of diabetes along with sick day(s) can get challenging. If left unchecked, things can escalate pretty quickly.
If you (or your child) have vomiting, diarrhoea and nausea, inform your doctor immediately
WHAT IS A SICK DAY AND WHY IS IT IMPORTANT TO MANAGE?
When you have any kind of an infection or illness (unrelated to diabetes too) you might have to make changes to your diabetes management to maintain your sugars in your target range. Out of control BG could lead to a various avoidable complications such as DKA and increase the recovery period.

Don't stop insulin
Whatever happens, do NOT stop insulin. If you are a T1 whose body doesn't produce insulin, lack of insulin is most definitely going to cause DKA (Diabetic Ketoacidosis) which can be life threatening if left untreated. Most illnesses are accompanied by a certain degree of insulin resistance, meaning BG would be higher than normal and you might need more insulin, even if you are eating less or not eating at all. In this case preferably increase your bolus rather than basal because once the illness and insulin resistance weans off, you'll land up in hypo with the increased basal unless you're using a pump and you can go back to your original basal immediately.
If you skip a meal (and your BG is normal), you could skip bolus (rapid acting insulin) for that specific meal but do not skip basal (long acting)
When BG is high and you want to skip a meal, take only a correction dose (not meal dose) to bring back BG to normal range. Some people may use intra-muscular injections to quickly correct high BG since this method works faster than subcutaneous shots. On the pump, you could play around with the temporary basal, if you need to.
Monitor blood sugars frequently
Check BG every 2-3 hours and act accordingly. An important point to note is that once BG is elevated, one becomes more insulin resistant that usual. That means that your usual correction factor may not be enough and you may need more bolus (be careful of insulin stacking). For those on the pump, if you have a stubborn high that refuses to come down and you think it could have to do with a malfunction of your pump or patch, it's best to take a correction on MDI (syringe/pens)
If you don't check BG more often than usual on a sick day, you won't know how you're doing so it's very important to test frequently. Sometimes haywire BG can be a signal from your body that you're heading towards an illness in a day or two. If possible, use a CGM/FGM in addition to your glucometer if it helps you test more often.
Remember, the probability of developing DKA is extremely low if your BG is under control.
Tip : Dr Bernstein's Law of Small Numbers is my favourite hack to maintain normoglycemia (normal, steady BG) through good health and illness.

Check for ketones
Make sure you have ketone strips with you. Definitely check ketones if sugars are over 250 mg/dl. You may notice fruity odour on the breath, that is one indicator of potential ketones. Do not treat ketones with more carbs+insulin. Have salty liquids and correct BG to the normal range.
High BG + dehydration + ketones = recipe for disaster
If ketones are present at normal BG, no need to panic - keep testing BG and ketones. Certain commonly taken medication such as asprin may cause false positive ketones, so it's good to keep that in mind when you're ill. We are trained to jump when we hear the word 'ketones'. Read this article to understand the difference between 'ketosis' and 'ketoacidosis'. Also know that technically diagnosing DKA is a clinician's job and we can't do it at home (all we can do at home is test for ketones, which are just one indication of DKA. There are many others like pH, anion gap, arterial blood gas, etc)
Hydrate/eat light
Ensure you drink enough fluids and top up with electrolytes (water, salted broth/soup, salted lemon+water, etc) since dehydration can turn dangerous. If you're okay to eat, you'll need something that's easy to make, good on the sugars and light enough to digest. When you lose fluids through vomiting or diarrhoea, these fluids need to be replaced. If fluids are not pushed intermittently, the concentration of glucose in the blood is going to steadily go up - and without enough insulin in the body, that could push you towards DKA.

Make a sick day plan
Sit down with your healthcare professional and develop a contingency plan for what to do when you are sick and keep printed copies with you, at home, work or school. Problems often come unannounced and it's best to be prepared. Here's our list of diabetes essentials you would want to keep in your dia-bag with you. Check your kit every few months to make sure it's up to date and restock things you might have used. For example, certain gastro issues tend to cause hypos for most people. Make sure you have your low blood sugar kit and glucagon at hand.
Treat the underlying illness
Apart from managing BG when you are sick, make sure you treat the problem. Whether you have a cold, flu, chickenpox or any other type of illness, ensure you receive medical attention. Contact your doctor early to avoid becoming more unwell and needing emergency care.
When you call your doctor, make sure you have handy a log of your latest BG, ketones, food, insulin dose and any other observations.

Inform close/loved ones
Especially if you live alone, make sure you inform your family, neighbours, colleagues or friends to check up on you. If possible, share your CGM data with someone who can alert you or call for help incase you are hypo or hyper and unable or too sick to help yourself.
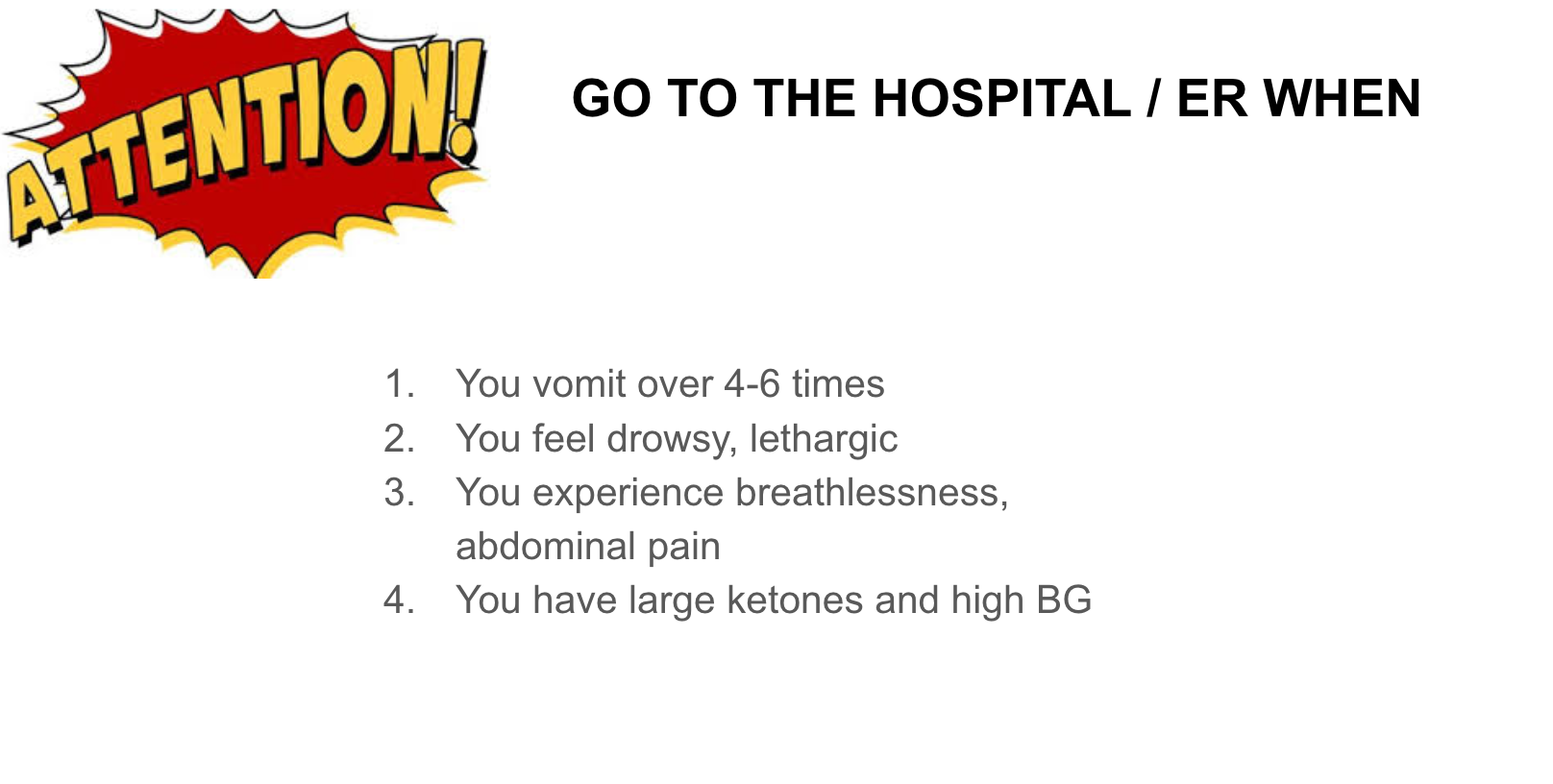
When in doubt and discomfort, call your doctor and go to the hospital. Treat it as a necessity and not a failure of your diabetes management. There will always be scope to learn and improve if you take a step in the right direction at the right time.
Stay happy, healthy and safe!
SUPPORT BLUE CIRCLE DIABETES FOUNDATION
We need your help and support to continue to grow, expand and touch the lives of countless people in the diabetic community. Every little bit helps us in sustaining this endeavour.
Click here to donate